Unlocking the Mystery of Coenzyme Q
Antioxidants are seen as something great for our nutrition and are sometimes bought in supplement form. However, we actually make Coenzyme Q (a type of antioxidant) inside our mitochondria – the powerhouses of our cells. Scientists from Germany did research to figure out how this helpful substance moves from the mitochondria to the cell membrane, protecting it and stopping it from dying.
Coenzyme Q is really important for our bodies because it helps to protect us from getting sick. It can prevent serious illnesses like Leigh Syndrome, which will make your muscles weaken and cause other bad symptoms. We need Coenzyme Q in our body even when we’re young – as early as 20 years old! But why can’t we just eat it?
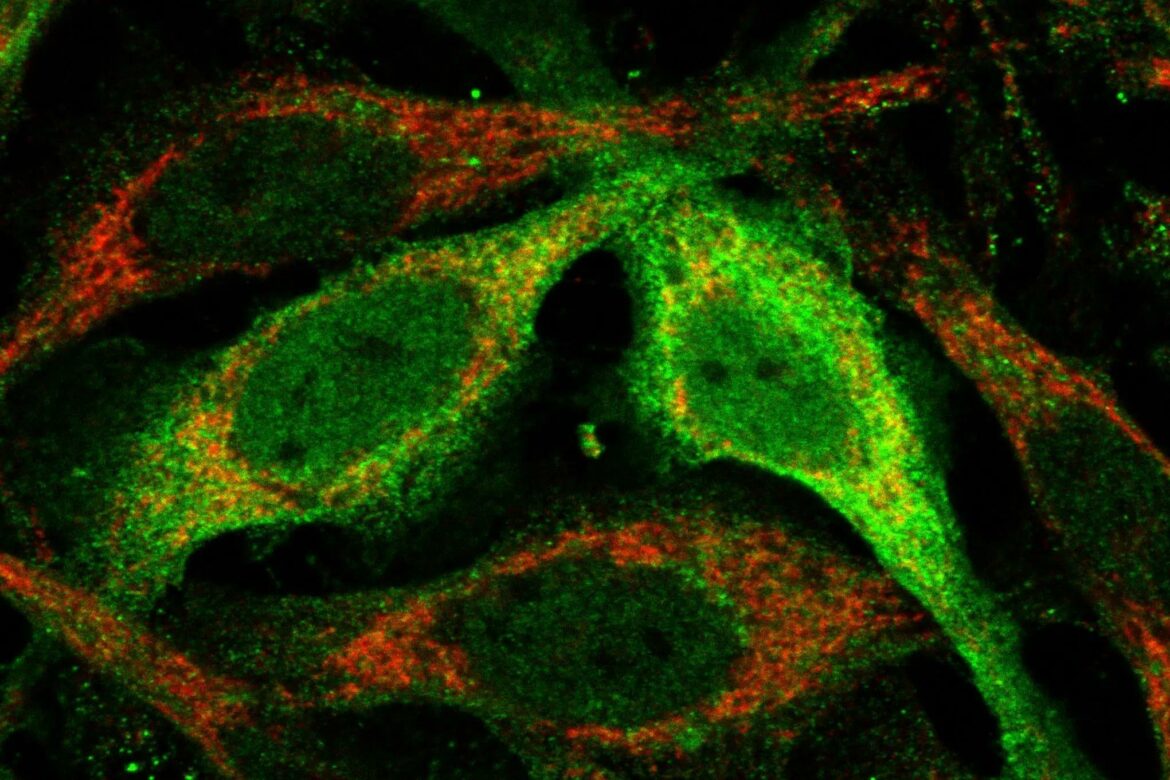
Soni Deschwal, a scientist from the Max Planck Institute for Biology of Aging says that our bodies don’t absorb Coenzyme Q very much from food. This ingredient is not soluble in water and can be found inside mitochondria. It’s an antioxidant that needs to pass through the wet and slimy cytoplasm in order to protect lipids (fats) from being damaged by oxidation.
Deshwal explains that their research has identified proteins in the cell which help to transport Coenzyme Q. Through their findings, they discovered an enzyme called STARD7 which is responsible for helping move this coenzyme between mitochondria and within the cytoplasm.
Mitochondria
The mitochondria are delivering special things to the cell walls – like band-aids! This helps keep cells healthy and prevents them from dying, according to Deshwal. The mitochondria do more than just provide energy for our cells – they play a very important role in keeping them safe too!
Scientists are doing research to figure out how to move a type of molecule called Coenzyme Q into the cells of someone who has a disease like Leigh Syndrome. If they can do that, it could help people with those diseases get better.
Scientists recently published a study investigating how mitochondria and enzymes work together to keep our eyes healthy. The research focused particularly on the role of conjunctiva goblet cells which aid in keeping the surface of our eyes in top condition.
Scientists are studying ways brain-derived neurotrophic factor could help treat retinitis pigmentosa, which is an eye disease caused by mitochondrial damage. They are also looking at how the expression of certain genes related to mitochondrial dynamics changes in a rat with glaucoma. Finally, they are researching a possible vaccine for human brucellosis that could be made from influenza viral vectors and testing it out on guinea pigs to see if they can come up with an immunization schedule.